Welcome to the Neurexpert Blog
Translating the Latest Neuroscience Research.
What has birth got to do with autism?
by Carolyn Lacey , 12 Aug 2015.
A prominent neuroscientist suggests that the trend towards greater birth interventions could be correlated with greater incidence of autism spectrum disorders. We discuss his reasoning in our latest blog post.
It’s the one thing that we all have in common: we are born.
Life outside the womb is a lot different to life inside. The brain, like the rest of the body, has to get ready to adapt. In this blog post I summarize an opinion piece published in Nature Neuroscience written by Yehezkel Ben-Ari, a professor at INMED France, on brain changes that occur prior to, and during birth, and how he postulates that hormones involved in birth may be associated with Autism Spectrum Disorders.
To date 1% of the population is diagnosed with Autism Spectrum Disorders world-wide. The number of diagnoses each year is steadily increasing with almost double the number of children diagnosed in 2010 compared to 2000 (one in 68 compared to one in 150 children; Centers for Disease Control and Prevention).
Why has the number of cases of ASD increased over the years? It could be due to increased awareness and better diagnostic criteria, or, maybe, as the article I am going to cover in today’s blog post suggests, it could be due to increases in birth interventions such as caesarian sections (now over a third of births in many countries; World Health Organization) and induction.
Let’s get to the science.
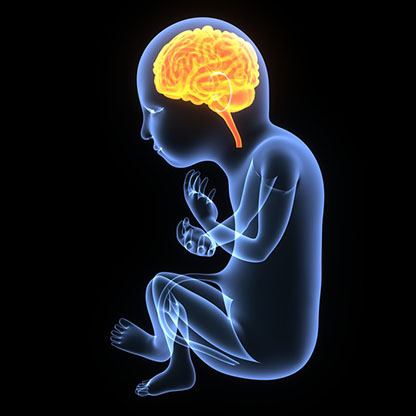
Autism develops in the womb
Autism Spectrum Disorders (referred to from now on as ASD) have a wide range of symptoms but are most commonly characterized by altered social interaction/ communication and repetitive behaviours (see link at end for more information).
ASD are neurodevelopmental disorders. This means that the disorder manifests as the brain is growing. Brain differences in ASD can occur during gestation at a time when neurons are: migrating to the right place in the brain; growing in number; and making connections with each-other. There does not seem to be one unifying cause of ASD in every person diagnosed and it is likely to be a combination of genetic and environmental factors that are important during brain development.
Keeping the brain in check
During brain development there are changes in operation known as critical periods or checkpoints. If a checkpoint is missed then the brain will not develop properly. For example, one checkpoint occurs upon eye-opening. If the eyes remain closed then the visual system will not wire correctly.
Cells in the brain communicate with each other through chemicals and electricity. Chemical and electrical communication in the brain work closely together and influence each other.
A major checkpoint in brain development involves a chemical called GABA (a type of neurotransmitter). Although it is not known when the GABA checkpoint happens in humans, it is thought to be sometime prior to birth. Before the checkpoint, GABA increases electrical signals (causing giant voltage changes) but, after the checkpoint, GABA decreases electrical signals.
Lots of electrical communication is great in the pre-birth brain as it helps neurons talk to each other and talking neurons means that they can make the correct connections for later function. But, once born, it is preferable to have less electrical signals that are more meaningful so that the brain can achieve more goal directed behavior such as reaching for a specific object. Too much electrical activity can have adverse effects like seizures.
The electrical activity generated by single cells combines to create synchronized activities, called oscillations, which help widespread regions of the brain to talk to each other. Cells that contain GABA are particularly important for generating the gamma oscillation (important when you are awake, doing high cognitive tasks such as problem solving, and dreaming; see blog from last month here).
Ben-Ari suggests that, in ASD brains, GABA continues to enhance electrical signaling, acting more like pre-checkpoint GABA. Indeed, children with ASD have been shown to have alterations in gamma oscillations and it is also interesting that one-third of children diagnosed with ASD also have epilepsy (seizures are characterized by too much synchronized electrical activity in the brain).
But what has this got to do with birth?
GABA checkpoint comes about partially because of a reduction in the amount of chloride ions in brain cells that contain GABA. Birth is stressful for both the mother and baby. Increased stress hormones change brain chloride levels. This pushes GABA towards pre-checkpoint behavior (more electrical signals). The labour hormone Oxytocin (also known for playing a role in love and bonding) can help reduce chloride ions and protect GABA from this set-back (and make sure it continues to reduce electrical signals). In other words, oxytocin, via chloride ions, could prevent GABA from being pushed into pre-checkpoint function by the stress hormones produced during birth. (Interestingly, newborn humans have extremely high levels of stress hormones not even seen in severely stressed adults.)
In his Opinion piece, Ben-Ari suggests ASD symptoms may be partially influenced by some disruption of the GABA checkpoint during the birth process. Perhaps oxytocin does not counteract the deleterious effects of stress on GABA function. In models of ASD, GABA continues to act to increase electrical signaling after birth and gamma oscillations are increased. There are a number of suggestions that this oxytocin-mediated protective mechanism may not occur in human ASD brains, such as the high incidence of epilepsy and alterations in gamma oscillations in children with ASD. In addition, children with ASD have lower levels of oxytocin.
Why care?
Over the last few decades there has been a trend towards an increase in medical interventions in the birth process (emergency caesarean section and induction) and also a “too posh to push” trend towards elective caesarean section. A small number of studies have identified a possible link between birth interventions such as caesarean section and the use of oxytocin to start or augment labor, as well as birth complications such as preterm birth and hypoxia, with risk of ASD. However, one of these studies also identified being born in the Summer with increased risk of ASD (see link at end)…
It is hard for me to reconcile how both less oxytocin (elective caesarean births) and more oxytocin (induction/ augmentation of labour) can lead to ASD. Although, maybe it’s all about having just the right amount of labour hormones. So, in my opinion, the jury is still out on whether birth interventions contribute to ASD risk.
To view the original paper discussed in this blog “Is birth a critical period in the pathogenesis of autism spectrum disorders?” in Nature Neuroscience please click here.
Links to related information:
http://www.cdc.gov/ncbddd/autism/data.html
http://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
http://www.cdc.gov/nchs/fastats/delivery.htm
http://www.who.int/healthsystems/topics/financing/healthreport/30C-sectioncosts.pdf
http://www.nejm.org/doi/full/10.1056/NEJMoa1307491
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3387855/
The Blog was written by Carolyn Lacey, Scientific Outreach Manager at Neurexpert. To learn more about Carolyn and Neurexpert, please click here.
Recent Blog Posts
Sleepless with the Enemy: how skipping sleep changes your social life and how dreams become reality
Ever stay up too late and wake up thinking the world is out to get you? We cover a new study that shows that sleeping and dreaming helps you read other people better. Skipping just one night of sleep makes your brain read threat in friendly faces and, in contrast, bigger dreams make for better reality.
Depressed? Suck it up!
Depression sucks and anti-depressants often don't work. Our latest blog sniffs out a new treatment published in Molecular Psychiatry that could be the future for #depression sufferers.
Stressed out of my mind
June 27th is Post-Traumatic Stress Disorder (PTSD) Awareness Day and so this blog is dedicated to neuroscience related to chronic stress.
Exciting times ahead at Neurexpert
Neurexpert appoints Dr Carolyn Lacey as Scientific Outreach Manager

Brochure Publications